The Thyroid Gland
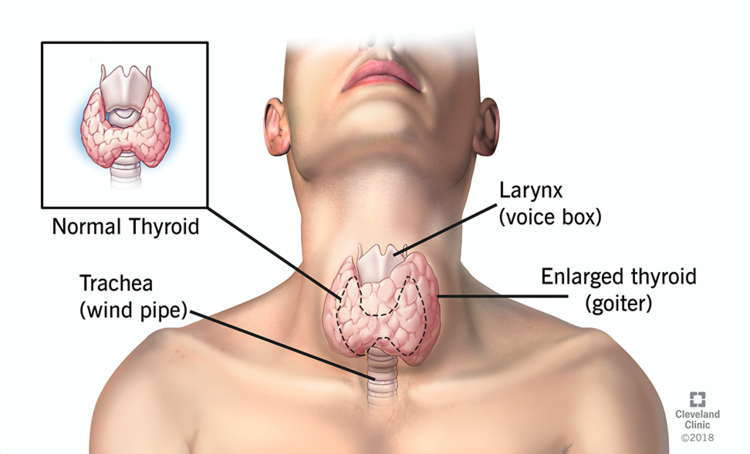
The thyroid is a butterfly-shaped gland located in the neck, surrounded by major vessels, the trachea (windpipe), and the larynx (voice box). The hormones the gland produces (most importantly T3 and T4) regulate metabolism. A third hormone produced by the thyroid, Calcitonin, regulates calcium in the body.
Because the thyroid regulates metabolism, it is also involved in the regulation of body weight and temperature, heart rate, alertness, growth, bowel activity, and menstrual cycles in women. Overactivity of the thyroid results in increased metabolism with weight loss despite an increased appetite, an increased heart rate, heat intolerance, shaky hands, and in some cases, an eye bulge. Symptoms often vary depending on the severity and the person.
An enlarged thyroid (Goitre) is usually visible in the mid-lower part of the neck. In some cases, the thyroid can grow down into the upper part of the chest cavity, where it won’t be visible to the outside.